Essentials of Breastfeeding
Congratulations on choosing to breastfeed your baby! Breastmilk is more than good nutrition. It is tailor made for your baby. Sometimes breastfeeding doesn’t go as smoothly as we would like it to or think it should. So after delivery take a deep breath, relax, and just focus on taking care of yourself and your baby – those dust bunnies under the sofa can wait. Here are a few essentials to keep in mind to get breastfeeding off to a good start.
What to do before the baby arrives.
Preparing your nipples.
You may have heard that your nipples need “preparing” prior to the birth of your baby to avoid sore nipples. This old wives’ tale had women scrubbing their nipples with a dry toothbrush, loofah, or washcloth. Research has shown that the only way to prevent sore nipples is good latch-on and positioning – not a loofah.
Read a good book … or a website.
Arming yourself with as much information about breast feeding before your baby is born will make it easier for you to understand the mechanics of breastfeeding. A few suggestions:
- A Nursing Mother’s Companion by Kathleen Huggins
- The Womanly Art of Breastfeeding by La Leche League International
- Nursing Mother, Working Mother by Gale Pryor
La Leche League:
Buy a nursing bra.
A bra specific for nursing is not necessary, but it may make it more comfortable for you and easier for baby to gain access when breastfeeding. A rule of thumb is to buy one cup size larger than you are during your 9th month of pregnancy and make sure the bra is made of cotton. Many moms find three bras work well: one in the laundry, one ready to wear, and one in action.
The baby’s here, now what?
Ideally you want to initiate breastfeeding about one hour after birth. Babies are very alert during this time. Even if latch-on is not successful, you’ve made an imprint. Next time, baby will recognize the smell, texture, and taste.
How often should I feed?
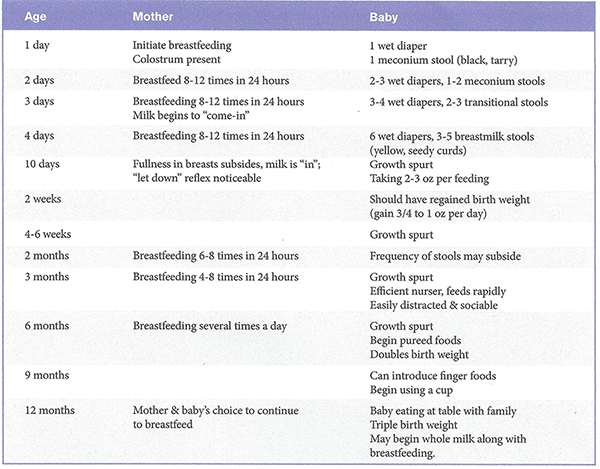
Research has shown that until breastfeeding is fully established, early and frequent feedings are best. Place your infant to the breast at least every two to three hours. You want eight to 12 feedings in 24 hours.
Sometimes babies will nurse more frequently at cer- tain times of the day. This is called cluster feeding. For example, perhaps your baby is feeding every one to two hours in the late afternoon and evening and then he does not nurse for four hours. After cluster feeding, babies tend to go into a deep sleep. This is perfectly normal.
After your milk supply is established, usually in about two weeks, feed baby on demand which is typically every three to four hours. If baby sleeps through the night, say “thank you baby,” but do not let him go more than five hours without a feeding.
How long per feeding?
Don’t get too hung up on how long to feed your baby. However, a good rule of thumb is to breastfeed at least 15-20 minutes on each side. Remember to alternate the breast you start with each time. Feedings are timed like contractions – from the beginning of one to the beginning of the next. It is not unusual for feedings during the first two weeks to take up to 40 minutes. When you are producing mature milk, and as your baby matures, feed ing may take only 20 minutes total. However, it’s impor tant for baby to empty the breast completely to make sure she receives the hind milk which is rich in fat and calo ries. (You will notice that your breast feels lighter after a feeding.) Sometimes babies will only nurse on one side and then fall sleep and you just can’t wake them up. This is normal. Just be sure to nurse from the other breast first at the next feeding.
Is baby getting enough?
This is a common question among all breastfeeding par ents. In the first couple of weeks, if your baby has six or more wet diapers per day and at least one stool (mustard colored and seedy looking), he is receiving a good supply of breast milk. (NOTE: Infrequent bowel movements are not normally seen until the second month oflife.) In addition, most babies will act satisfied after completing a feeding. Your baby should be back to birth weight by 10-14 days of age if breastfeeding is going well. T here fore, the two-week checkup with your baby’s healthcare provider is very important.
- Baby nurses 8-12 times/24 hours
- One wet diaper 1st day oflife, three on days 4-5, at least six thereafter
- Baby has a moist mouth
- You hear frequent swallowing (rhythmic suck/pause/ suck pattern)
- Yellow, seedy, loose stools on day 3-4
- Baby is satisfied after feedings
- There is tugging at the breast that is not painful
- You feel “after pains” (your uterus is contracting)
- You may feel let-down
- Milk may leak from the opposite breast while feeding
- Breasts are softer after a feeding
Letdown
Letdown (or milk ejection reflex) is when the milk moves forward in the breast toward the nipple and into baby’s mouth. It develops in about two to three weeks after birth and feels like “pins and needles.” In some women, particularly if this is your first baby, the let down reflex can be quite painful. Be assured that this should subside when your baby is about a month old. It may be helpful to perform your breathing exercises that you learned in childbirth class.
Many times letdown occurs in the opposite breast while you’re nursing. Sometimes letdown occurs when you hear your baby cry (or someone else’s baby) or are just thinking about your baby. This is called leaking. It may be helpful to use nursing pads to absorb the milk. Change the pads frequently to keep your nipples dry.
Supplemental bottles
Do not offer your baby any bottles during the first three weeks after birth. Good lactation depends on frequent emptying of the breasts. Supplemental bottles take away from nursing and reduces milk production. If you are concerned that your baby is not getting enough to eat, consult with your healthcare provider or a lactation con sultant.
After your baby is three weeks old and breastfeeding is well established, you may want to offer your baby a bottle of expressed milk once a day so that they can become accustomed to the bottle and artificial nipple. It may help the baby to accept the bottle if someone other than the breastfeeding mother offers the bottle.
Growth spurts
You should know that babies have growth spurts around day 10-14, at six weeks, and again at three and six months. During this time, because baby is feeding very frequently, many mothers are concerned that they don’t have enough milk for their baby. In fact, what baby is doing by nurs ing so often is increasing the supply so that in about 24 hours she will have a sufficient amount of milk to help her through the growth spurt.
Call your pediatrician or lactation consultant if:
- Baby has less than six wet diapers and less than one stool in 24 hours after the 4th day of life.
- Your milk has not “come in” by postpartum day five
- You have painful engorgement or sore cracked nipples
- You need to take a medication
- Your baby doesn’t seem to be gaining weight adequately
- Baby refuses to nurse
- Any questions or concerns
Don’t wait to seek help if breastfeeding is not going well. Don’t let frustration get in the way of a good breastfeed ing experience. Breastfeeding problems can be quickly and easily resolved if corrected early.
Enjoy this special time with your baby. By choosing to breastfeed, you have made a wise healthcare decision for you and your baby.