What is cervical cancer screening?
Cervical cancer screening is used to find abnormal changes in the cells of the cervix that could lead to cancer. Screening includes the Pap test and, for some women, testing for a virus called human papillomavirus (HPV) (see “Cervical Cancer Screening“).
What causes abnormal cervical cancer screening test results?
The main cause of cervical cancer is infection with HPV. There are many types of HPV. Some types have been linked to cancer of the cervix, vulva, vagina, anus, and penis. Some also can cause cancer of the head and neck. These types of HPV are known as “high-risk” types. Most cases of cervical cancer are caused by just two high-risk types of HPV—type 16 and type 18. Cells that are infected with HPV appear different from normal cells under a microscope. Abnormal changes can be mild, or they can be more serious. The more serious changes can lead to cancer if not treated (see “Human Papillomavirus [HPV] Vaccination“).
What is the difference between the terms cervical intraepithelial lesion and squamous intraepithelial lesion?
These terms are used to describe changes in the cervix, but they are used in different situations. Squamous intraepithelial lesion (SIL) is used to describe Pap test results. “Squamous” refers to the type of cells that make up the tissue that covers the cervix. SIL is not a diagnosis of pre-cancer or cancer. The Pap test is a screening test. It cannot tell exactly how severe the changes are in cervical cells. A cervical biopsy is needed to find out whether pre-cancer or cancer actually is present.
Cervical intraepithelial lesion (CIN) is used to report cervical biopsy results. CIN describes the actual changes in cervical cells. CIN is graded as 1, 2, or 3. CIN 1 is used for mild (low-grade) changes in the cells that usually go away on their own without treatment. CIN 2 is used for moderate changes. CIN 3 is used for more severe (high-grade) changes. Moderate and high-grade changes can progress to cancer. For this reason, they may be described as “precancer.”
What are the different types of abnormal Pap test results?
- Atypical squamous cells of undetermined significance (ASC-US)—ASC-US means that changes in the cervical cells have been found. The changes are almost always a sign of an HPV infection. ASC-US is the most common abnormal Pap test result.
- Low-grade squamous intraepithelial lesion (LSIL)—LSIL means that the cervical cells show changes that are mildly abnormal. LSIL usually is caused by an HPV infection that often goes away on its own.
- High-grade squamous intraepithelial lesion (HSIL)—HSIL suggests more serious changes in the cervix than LSIL. It is more likely than LSIL to be associated with precancer and cancer.
- Atypical squamous cells, cannot exclude HSIL (ASC-H)—ASC-H means that changes in the cervical cells have been found that raise concern for the presence of HSIL.
- Atypical glandular cells (AGC)—Glandular cells are another type of cell that make up the thin layer of tissue that covers the inner canal of the cervix. Glandular cells also are present inside the uterus. An AGC result means that changes have been found in glandular cells that raise concern for the presence of precancer or cancer.
Click on the FAQs below to expand
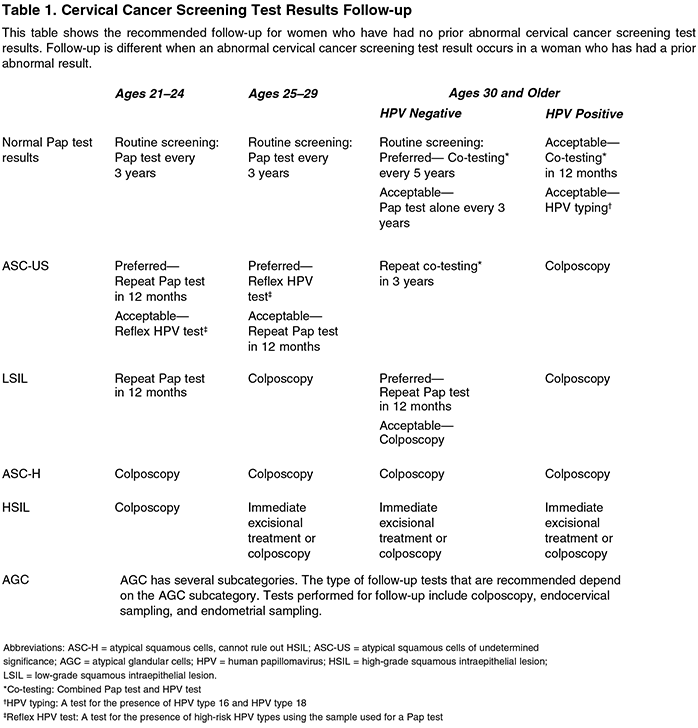
What testing is needed after an abnormal cervical cancer screening test result?
If you have an abnormal cervical cancer screening test result, you may need further testing. The following tests may be done depending on your age and your initial Pap test result:
- Repeat Pap test or co-test—A repeat Pap test or a repeat co-test (Pap test and a test for high-risk types of HPV) is recommended as a follow-up to some abnormal test results. These repeat tests may be done in 1 year or in 3 years depending on your initial test result, your age, and the results of previous tests.
- HPV test—An HPV test looks for the presence of the HPV types that have been linked to cervical cancer. An HPV test can be done on the same cells used for the initial Pap test. This is called reflex HPV testing. There is another kind of HPV test that looks specifically for HPV type 16 and HPV type 18. These two types cause the most cases of cervical cancer. This kind of HPV test is called HPV typing.
- Colposcopy, biopsy, and endocervical sampling—Colposcopy is an exam of the cervix with a magnifying device. If an area of abnormal cells is seen, your health care provider may decide that a cervical biopsy is needed. For a biopsy, the health care provider removes a small sample of tissue and sends it to a lab for testing. The lab tests can determine whether CIN is present and, if so, what grade it is. Endocervical sampling also may be done. A small brush or other instrument is used to take a tissue sample from the cervical canal.
- Endometrial sampling—A sample of the endometrium (the lining of the uterus) is collected for study. Some women with an AGC result need to have this follow-up test.
How are abnormal cervical cells treated?
In general, there are two ways to treat abnormal cervical cells: 1) “excisional” treatment and 2) “ablative” treatment. With excisional treatments, tissue is removed from the cervix and is sent to a laboratory to be studied. Results can tell whether CIN actually is present and, if so, how severe it is. With ablative treatment, abnormal cervical tissue is destroyed, and there is no tissue to send to a laboratory for study.
What types of excisional treatments are there?
Excisional treatments include the following:
- Loop electrosurgical excision procedure (LEEP)—A thin wire loop that carries an electric current is used to remove abnormal areas of the cervix.
- Conization—A cone-shaped piece of the cervix that contains the abnormal cells is removed.
What types of ablative treatments are there?
Ablative treatments include the following:
- Cryotherapy—An instrument is used to freeze abnormal cervical tissue, which then sloughs off.
- Laser therapy—A focused beam of light is used to destroy abnormal cervical tissue.
Glossary
Cells: The smallest units of a structure in the body; the building blocks for all parts of the body.
Cervical Biopsy: A minor surgical procedure to remove a small piece of cervical tissue that is then examined under a microscope in a laboratory.
Cervical Intraepithelial Neoplasia (CIN): A term used to describe abnormal changes in the cells of the cervix that are caused by infection with human papillomavirus. CIN is graded as 1 (low-grade), 2 (moderate), or 3 (high-grade).
Cervix: The lower, narrow end of the uterus at the top of the vagina.
Colposcopy: Viewing of the cervix, vulva, or vagina under magnification with an instrument called a colposcope.
Conization: A procedure in which a cone-shaped piece of tissue is removed from the cervix.
Cryotherapy: A freezing technique used to destroy diseased tissue; also known as “cold cautery.”
Human Papillomavirus (HPV): The name for a group of related viruses, some of which cause genital warts and some of which can cause cancer of the cervix, vulva, vagina, penis, anus, mouth, and throat.
Loop Electrosurgical Excision Procedure (LEEP): The removal of abnormal tissue from the cervix using a thin wire loop and electric energy.
Pap Test: A test in which cells are taken from the cervix and vagina and examined under a microscope.
Squamous Intraepithelial Lesion (SIL): A term used to describe abnormal cervical cells detected by the Pap test.